Margins in Breast Cancer
What about Margins in Breast Cancer
Margins in breast cancer are important for any surgery because the entire tumor needs to be totally removed. During a work up prior to surgery, one very important question for breast surgery is “can this lesion be resected with a limited procedure or is a total mastectomy required?” The total tumor removal is mandatory for cancer surgery which is obvious. Then the question becomes how much clear margin is present?
The margin analysis is different for total mastectomy vs. a limited resection or lumpectomy.
The total resection (mastectomy) takes all of the breast, leaving the chest wall as a large margin. Most often this deep margin is covered by the remaining chest wall/breast skin that is sewn together as a primary closure by the surgeon. The main concern is the deep margin of the mastectomy specimen. The superficial margins are also analyzed but usually if the tumor is superficial, the surgeon will leave breast skin in place to cover the tumor. Both superficial and deep margins are important; we tend to focus more on the deep margin and careful attention is mandatory, requiring visual inspection and palpation for any subtle abnormality. Any suspicious area should be sampled and examined microscopically for tumor presence. The deep tumor free margin is measured in millimeters.
The lumpectomy takes a portion of breast tissue containing the tumor, and leaves behind breast tissue on all sides of the resection. In a previous blog, I discussed the importance of measuring the tumor accurately. The other measurement that is important with lumpectomies are the margins. Since this limited resection in general comes for the “middle” of the breast, it leaves behind margins from 360 degrees. So, all margins in a lumpectomy specimen are the distance from tumor to native breast tissue left behind. We designate 6 sides of the lumpectomy as superior, inferior, anterior, posterior, medial and lateral. Each side has a different color ink applied that survives fixation, slicing, and slide making. Since all of the lumpectomy specimen is typically sliced and submitted, all margins can be assessed for nearby tumor. The colored ink represents the surgical margin.
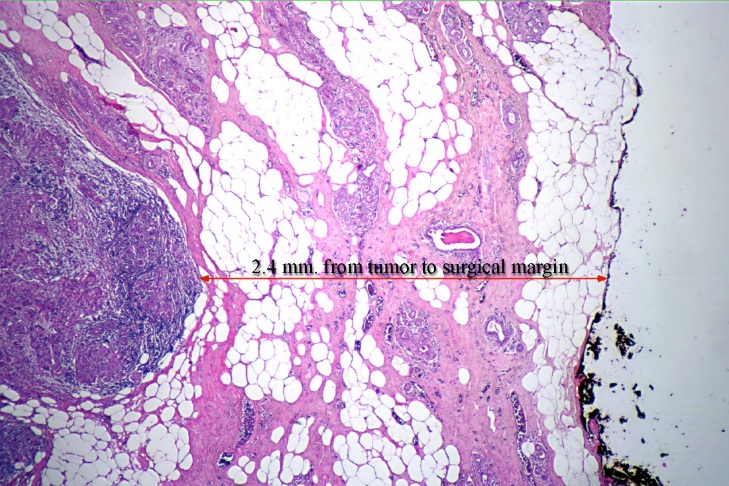
The image to the left demonstrates a microscopic measurement of a surgical margin. In the center on the left side is tumor forming a dense cellular area of invasion (dark area) toward the surgical margin. To the far right of the tissue, ink marks the surgical margin. In between the tumor extension and the surgical margin is normal breast tissue. The distance between the tumor and inked margin represents a free zone or clear margin that measures 2.4 mm. This represents a close but clear margin.

To get an idea how small a single millimeter is, think of a penny. It is 19 mm in diameter.
As discussed above, margin analysis is different for mastectomy and lumpectomy specimen. Furthermore, acceptable margins differ for invasive and non-invasive disease, with greater clear margin distance preferred for non-invasive disease (to be discussed in later blog). Malignant tumor at the inked surgical margin is not acceptable. The decision on acceptable margins are usually decided by the breast team after careful review of the literature. My experience is that the standards on adequate margins change from time to time.
The next blog will further discuss the approach to margins with respect to the type of resection (mastectomy vs. lumpectomy) and the type of breast cancer diagnosed.
North Houston Pathology Associates takes great care in measuring these margin distances. Pathologists who attend the weekly breast conference learn how important these measurements are to the breast team members, especially the breast surgeons, medical and radiation oncologists. Patients are the ultimate beneficiaries.