How Important Is Communication Between Physicians
How important is communication between physicians?
This is a silly question because everyone knows the answer; but how often is it practiced effectively?
When we began our comprehensive breast program in early 1996, the breast center and the pathology department were separate and although on the same first floor, we were basically on opposite sides of the community hospital. As we learned early on as the breast center ramped up, the communication between the mammographer and pathologist was critical if we were going to achieve the excellence that we had promised our patients.
Since our departments were not “next-door-neighbors,” walking over to discuss a case was not realistic, nor was phoning back and forth: both specialists were busy and often not available to talk on the phone about a biopsy. Quickly we developed a WORKSHEET. It was a digital production using Microsoft Publisher and was easily edited as desired. From its inception, this worksheet was to encompass most mammographic issues as a checklist easily filled out by the mammographer or by a tech as directed by the mammographer. It was meant to be easily filled out and submitted to pathology with the biopsy container and other requisition forms.
We knew that concordance was an important issue and this worksheet helped ensure that the purpose of the biopsy itself was conveyed clearly to the pathologist. The pathologist’s part of the worksheet was limited to positive, indeterminant or worrisome, or negative for malignancy. The issue of concordance was later determined by the mammographer when he/she reviewed the biopsy surgical pathology report. If the mammographic suspicion was confirmed after reading the pathology report, then there was concordance. If there was no agreement, there was no concordance and further studies would ensue after consulting with the referring physician.
Below is an example of a worksheet.
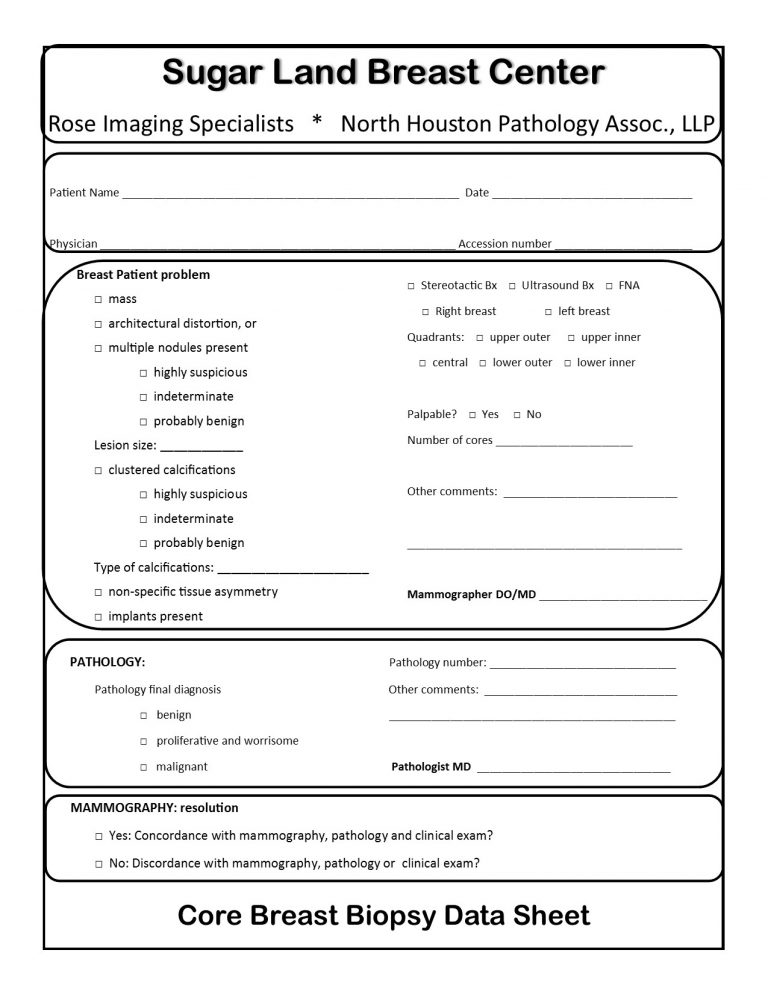
We began using this worksheet in early 1996 and have used it ever since. Using Microsoft Publisher, it can be modified if more check points need to be added or if a new breast center is opened. Most of this worksheet is filled out in the breast center and the patient problem check list is filled out by the mammography team and signed by the mammographer. This form accompanies the biopsy container and submission papers to pathology. When the stained slides of the biopsy tissue are given to the sign-out pathologist, this form accompanies the typed gross dictation. Once the pathologist makes his/her final diagnosis, this form is filled out and sent back to the breast center with the pathology report. Concordance is assessed by the mammographer after reviewing the mammographic images and report, and the pathology report.
This communication system has worked very well for our breast center over the past 20 plus years.