What else happens at the weekly breast conference?
What else happens at the weekly breast conference?
Our breast team began weekly prospective meeting in early 1996. We had recently attended a Laszlo Tabar Interdisciplinary Conference in the Palm Springs area in late 1995 and decided we wanted to expand our services to women coming to our breast center. The beginnings were not grand because we had to put together presentation equipment for both radiology as well as pathology. That did not take away from the enthusiasm of beginning our own weekly breast conference.
It is a common understanding that these weekly, prospective breast meetings are a powerful way to practice breast care in a complex setting, either in a hospital breast center, or a free-standing breast center. We met every Friday at 12:30 PM with the hospital providing lunch. Typically, patients with recent biopsy results were the majority of cases presented. Each case was presented first by the surgeon who detailed the complaint and physical findings. Next the mammographer presented pertinent mammographs and sonogram images and when appropriate discussed the estimated extent of disease. Finally, the pathologist presented a few images of the malignant or borderline disease and a synopsis of the pathology report. Then the discussion was opened up to other surgeons in attendance, with commentary from medical and radiation oncologists as appropriate. Sometimes plastic surgeons attended also.

Once you have attended a breast conference with active participation, you will never want to miss another one, and you will realize how incredibly useful the ensuing discussion is in determining the final management of each breast cancer patient. In these conferences, the individual patient’s wishes are carefully discussed together with the scientific discussion on the extent of the disease, the classification of the malignant process, and the hormone receptor and Her2 status of the tumor cells. The give and take amongst these specialists who treat breast cancer patients is often lively with the purpose of achieving the best recommendation for treatment for each individual patient.
Along the way, something else happens at breast conference: learning about microscopic diagnostic details as well as insights into pathology lab methodology. To this old pathologist, it is easy to add an interesting photograph that explains questions asked during conference or elsewhere—maybe in the hallway or at lunch. Some examples are below as links.
Many times, in conference or in a phone call from an impassioned mammographer, there is the comment that the pathologist lost the calcifications that were clearly in the post-biopsy specimen radiograph. We struggle with these accusations and if we are careful, we can usually explain the discrepancy.
Since we use a worksheet that that is filled out in mammography with lots of information on the patient and why the biopsy was performed, we already know why the biopsy was done before we look at the glass slide. This worksheet describes the problem(s) mammographically and actually accompanies the histology slide to the pathologist’s desk.
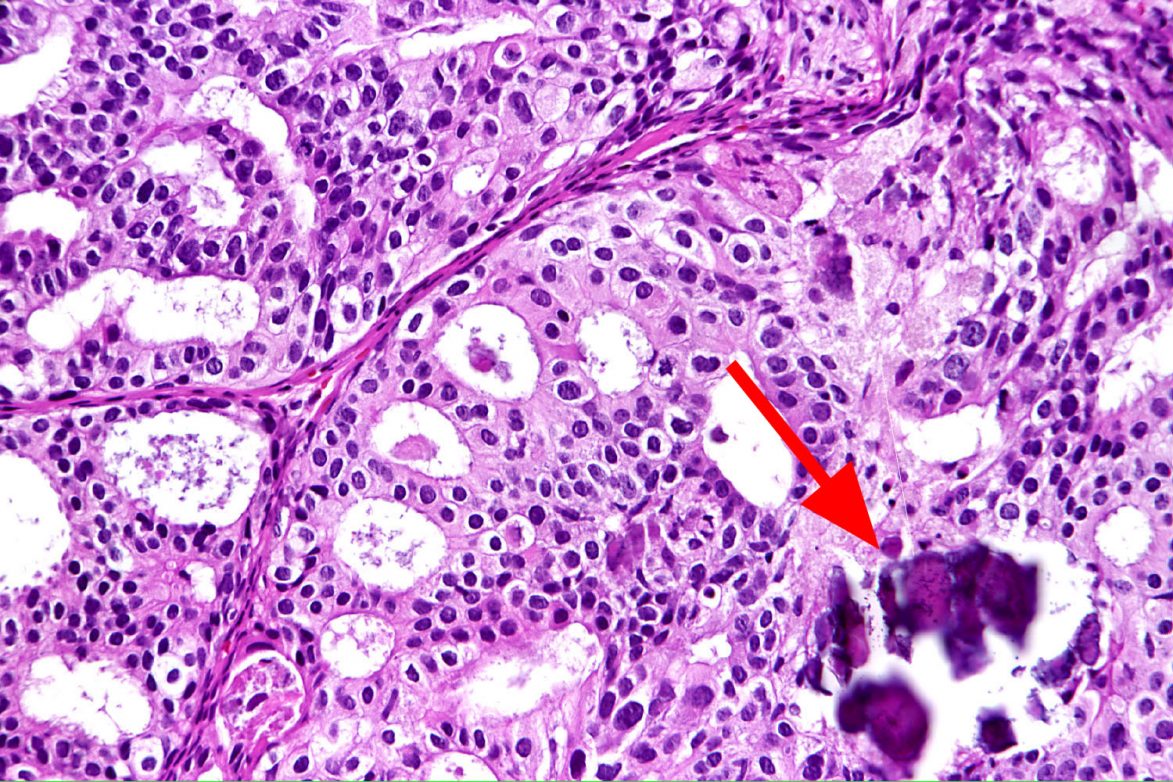
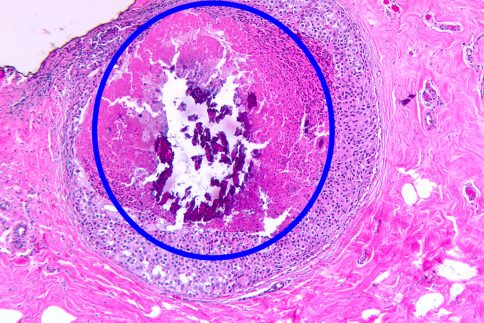
So, in the case of microcalcifications, we know in advance that we need to do a very careful search for calcifications and search for where these calcium deposits are located. Typically, three slides with multiple levels are cut for the initial microscopic review. If macrocalcifications are not found on routine cut slides, deeper levels are cut. Sometimes cutting through the entire paraffin block is carried out so that the entire specimen is examined under the microscope. Of course, examination under polarized light for calcium oxalate deposits is routinely performed.
One of the most common findings is that the sharp knife of the microtome, that cuts the ultra-thin tissue sections, actually catches the tip of the calcium deposit and flicks it out of the tissue slice. We have examples of how most of the calcification is fractured and pops out of the tissue section. (Please see above images).
Surgeons have taught us how to improve our report by including a comment regarding how many calcifications are located in malignant disease and how many are located in benign disease. This kind of pathologic reporting is very useful when the surgeon talks with the patient who knows there are abnormal calcifications in her breast. Sometimes the decision after biopsy reveals malignancy is whether to attempt a local excision or lumpectomy, or mastectomy. If the surgeon knows in advance that there are calcifications associated with benign disease and the malignancy, or benign disease only, the surgery he/she can recommend to the patient is much better calibrated with this knowledge beforehand.


The above is a lesson the pathologists learned from the surgeons. And this lesson was learned in the weekly comprehensive breast conference. I must interject that this lesson of stating clearly how the calcifications were distributed in the biopsy tissue is an important lesson for pathologists. We learned that this statement of clarity regarding microcalcifications benefits patients and the treatment they receive in this comprehensive setting. If at least one pathologist always attends breast conference, the opportunity for improvement via “cross-pollination” won’t be missed.
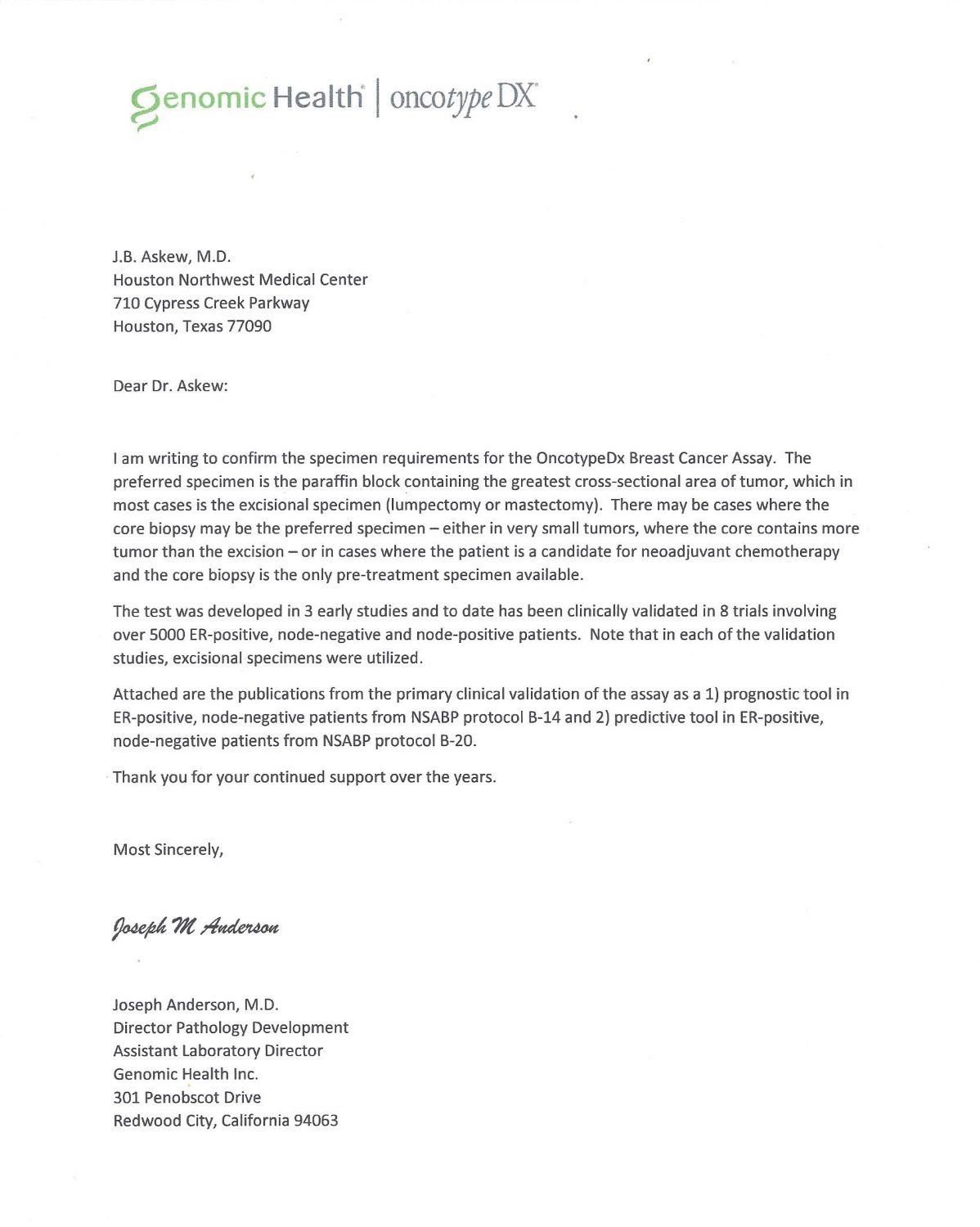
Several years ago, we noticed certain MDs were ordering one of the predictive multiple gene tests on biopsies. Since we reviewed each order so that we could select the best paraffin block for this expensive test, we were surprised to see the order came for the core biopsy and not from the lumpectomy/mastectomy specimen. Further inquiry into this request, we learned the physician had the idea that the needle biopsy actually disturbed and changed the genetics of the tumor (thought the DNA was changed by the needle passing through it), so that the only “undisturbed” tissue was the biopsy itself. As pathologists, we thought this reasoning was not scientific and so consulted the lead pathologist at the testing laboratory. This well-known pathologist confirmed that the optimal specimen is one taken, according to protocol, from either a lumpectomy or mastectomy specimen.
This extra effort on the pathologists’ part to optimize specimen collection is something that can be discussed in the weekly breast conference. The participating clinicians need to know about best practices even if it involves pathologist’s specimen collection, i.e. picking the best paraffin block for testing. Since we submit all of the tumor in lumpectomy cases, (and many sections in mastectomy) there are plenty of tissue blocks to choose from when the gene testing is ordered. In contrast, a gene test ordered on a core biopsy specimen, may have diminishing tissue available after levels have been cut for diagnosis (usually 3-6 levels) then more levels are needed for ER & PR, and even more levels for Her2 if the tumor is invasive. The wisdom of selecting the optimal specimen is obvious and something pathologists do gladly. Ultimately, the patient benefits from the test being performed on the optimal specimen. This topic is easily discussed during the weekly conference, during or after presentations.
When we process breast tissue, especially core biopsies, tissue fixation is very important and sometimes can delay the final diagnosis. The CAP (College of American Pathology) issues guidelines on the minimum amount of time required for fixation of the core biopsies in order that subsequent marker tests such as ER. PR and Her2neu are performed on properly prepared tissue, meaning optimal fixation.
When a pathology lab participates in a comprehensive breast center(s), it is imperative that the results are available as soon as possible. We endeavor to process a Monday breast biopsy beginning on the same day, and in most cases, will have a definite diagnosis by the next day, Tuesday. Now this rapid turn around time is predicated on proper fixation. So, this requirement of six hours fixation means the biopsy must reach the lab in time for six hours fixation before overnight tissue processing. The needle biopsy clinics know the cores must be taken and in formalin by 2PM each day for next day results. If the cores are placed in formalin later than 2 PM, the cores will be held overnight, with processing to begin on Tuesday and results out the next day, Wednesday.
These optimal requirements for fixation and the reasons are easily discussed at the weekly conference. Once the clinicians know the pathology group is working for the best testing results for their breast cancer patients, they become grateful for the extra attention we pathologists perform for their patients.
We believe that engaged pathologists can add a lot to the weekly breast conference by taking a little extra time to educate the clinicians in the workings behind the scenes in the pathology laboratory. Even as you are showing images of a high-grade DCIS or invasive breast carcinoma, you can add one or two other photographs that shows a curious finding and it adds to the presentation. Those little extras showcase the pathology lab and those who work in the windowless rooms.
A little humor can spice up a breast conference. Make sure you know your audience. Subtlety works, and grossness doesn’t. The rest is left to your creative imagination. Humor is like garlic: escargot is so much better with it.
For a pathologist to be successful in a comprehensive breast center setting, 1. one must be accurate; 2. we recommend showing malignant tissue to another pathologist for confirmation; 3. always be available to your clinical colleagues, even well after 5PM; 4. and to support all of the people working in these high stress positions: secretaries and histotechs in pathology, and mammo-techs and ultrasound techs in radiology. The comprehensive breast center relies on a team effort and support of the team members keeps it running smoothly and with invaluable enthusiasm.